HHS Communications in the Early Days of the Pandemic
Records released in response to American Oversight's request for communications of officials at the Department of Health and Human Services. The responsive records span the early days of the pandemic, from January to March.
Records released in response to American Oversight’s request for communications of officials at the Department of Health and Human Services. The responsive records span the early days of the pandemic, from January to March.
Details on what is in these records are below.
Records received in October 2020
Records received in November 2020
Records received November 2020 to January 2021
Records received from December 2020 to February 2021
In these documents
Early Cases
Feb. 10, 2020: The Secretary’s Operations Center circulated an email saying that one of the Miramar cruise ship passengers, who had been evacuated from Wuhan, China, five days prior, had tested positive for Covid-19. This was forwarded to Brett Giroir, assistant secretary for health at HHS, and Sylvia Trent-Adams, the principal deputy assistant secretary for health. Giroir replied, “Oh boy!”
March 16, 2020: Trent-Adams sent an email discussing the fact that an individual had been tested for Covid-19 at Walter Reed Medical Center and was awaiting results while being seen by a staff physician. Just a few days before this email was sent, the president and vice president had been exposed to the coronavirus, but the White House said neither of them would be tested.
Early Confusion and Problems
Jan. 30, 2020: Ken Rapuano, the assistant secretary of defense, emailed Robert Kadlec, the assistant secretary for preparedness and response at HHS, referencing a meeting about which he said he was “receiving multiple feeds and they’re not all consistent.” Kadlec responded, “[Undersecretary of Defense James] Anderson represented DOD […] and I am not sure he may have heard or gotten all that transpired in the room or heard what was tasked because it was fairly vague. The dilemma is the State is looking to move 700+ all at the same time. That was a shocker and one that we had not anticipated.”
Feb. 10, 2020: Giroir replied to an email with the subject line “Possible SG Activity – PREVENTS” saying “Why is the [surgeon general] involved? I guess it is fine of course, but has he done any work on this???” Steven Valentine, the deputy assistant secretary for health, responded, “They have proactively been reaching out to him – my impression is they want ‘the Surgeon General’ for PR.”
Feb. 13, 2020: Stephen Lindstrom, team lead for the CDC’s Respiratory Viruses Diagnostic Laboratory, emailed Mark Perkins, the World Health Organization’s chief scientific officer, asking who the point of contact was for Covid-19 testing at Japan’s National Institute of Infectious Diseases: “Sorry if someone from CDC has already reached out to you, but we are working to coordinate testing and repatriation of US citizens on the cruise ship in Yokohama and would like to learn more about the test they are using.” Perkins replied with the contact information for Makoto Takeda, whom Lindstrom then reached out to with a similar message. The Americans aboard the Diamond Princess were repatriated just a few days later, on Feb. 17.
March 14, 2020: Shayne Brannman, the project director at the Office of the Assistant Secretary for Preparedness and Response within HHS, circulated an email discussing the problems facing hospitals. She wrote that “CDC guidance for healthcare providers is not being followed consistently across hospitals,” that “PPE is being rationed at many locations,” and that “healthcare providers are being denied tests even when they have cared for suspect patients and are symptomatic themselves with fever, etc. They are concerned that they may be carrying the virus home to their children and elder parents. […] It is daunting how much PPE is needed for a 300-400 bed hospital.”
March 16, 2020: A 70-year-old nurse who had direct contact with repatriated Covid-positive patients in Miramar, Fla. said that she was denied a coronavirus test. She emailed Giroir; Kevin Yeskey, a principal deputy assistant secretary at HHS; and Christine Collins, the director of HHS’s Office of Emergency Management and Medical Operations with her complaint. Because of redactions over ensuing communications among the officials, it’s unclear whether she was ultimately able to get a test.
March 16, 2020: Kadlec sent an email saying that “demand for flu testing has dramatically increased diverting swabs available from COVID testing.” He continued, “We need to speak [to the] medical and public health community … to STOP testing for flu! We are burning both swabs and PPE.”
Early Recommendations to Mitigate the Virus’ Spread
Jan. 24, 2020: An email exchange between Giroir and Mia Heck, Giroir’s director of external affairs, had the subject line “WH meeting with POTUS on ends.”
Feb. 27, 2020: Carter Mecher, a senior adviser for the Office of Public Health in the Department of Veterans Affairs, circulated a “list of actions to take now” at the request of Kadlec. This included giving patients surpluses of their prescriptions so they wouldn’t have to go to health-care facilities for refills, moving up semi-elective procedures, establishing separate triaging and treatments for patients with potential respiratory illness, and caring for health-care workers.
Duane Caneva, chief medical officer at the Department of Homeland Security, responded, “We’ll take a stab on detention facility (congregate setting) actions, since ours is a real mess (250 federal, state, county prisons, jails, facilities that constantly mix international detainees around the nation—apparently it’s a secret sauce for disease spread).”
Also on Feb. 27, Michael Callahan, a doctor at Massachusetts General Hospital and special adviser to Kadlec’s office, circulated recommendations for the U.S. federal response to Covid-19, including a cohort system for health-care workers, care for health-care workers’ families, a medical device system, and greater oversight of the Biomedical Advanced Research and Development Authority. He also claimed that federal agencies were suffering from “painful, ineffective, and slow” communication and lack of individual initiative.
Kadlec forwarded these recommendations to Giroir, saying, “For your review. We will refine and finalize but want your initial impressions and comments today.”
March 12, 2020: Callahan sent an email to multiple doctors at Massachusetts General Hospital, as well as Kadlec and Giroir, proposing to “put the best of our US ICS-trained mass casualty infectious disease experts together” and “add to the non-federal voice that is getting the word out nationwide.” He said the issue was that “[m]edical system preparedness in the US is moving too slow compared to the propagation of the virus.”
PPE and Testing Shortages
Feb. 14, 2020: There was an email chain with the subject line “Potential Option For Infected/Mild Cases- Clinical Pharmacology Inpatient Study Units.” Rick Bright, who has now resigned from his post at the National Institutes of Health, asked if NETECs (regional resource centers of the National Emerging Special Pathogen Training and Education Center) were available or whether they were already filled. Kevin Yeskey, the principal deputy assistant secretary for preparedness and response, replied, “Those sites just don’t have the capacity.”
March 5, 2020: Roman Terrill, vice president at biotech company Integrated DNA Technologies (IDT), sent an email with the subject line “Urgent 40 minute warning from IDT on ability to ship tests-3 day pause likely!!!” There were many responses, including from Giroir and officials at the FDA, but they are redacted.
March 10, 2020: Anne Schuchat, the principal deputy director at the Centers for Disease Control and Prevention, discussed testing supply issues in an email to a California health department official. She wrote, “National shortage of the [Qiagen, a major provider of testing technologies] extraction components – request to Qiagen to send letter to cdc about comparability of their research use only products vs. good manufacturing products as a means to let us get FDA to permit those products being shipped out to fill the gap. We have not gotten that letter so this is in that company’s hands.” Schuchat continued, “Labs could try to use a different platform … which does not rely on those Qiagen products. Some places are pursuing that route. I don’t have info yet if any of the CA Counties are close to being able to do that.” At the time, testing shortages were a major problem in California.
March 11, 2020: Steve Monroe, director of the CDC’s Office of Laboratory Science and Safety, emailed Scott Becker, the CEO of the Association of Public Health Laboratories, asking, “Given the supply chain issues with extraction kits, do you know how many / which [public health labs] have one, or more, of the high-throughput extraction platforms currently cleared for influenza testing?” Becker replied, “I will see what information we have on this.” Giroir then said, “Let’s stay in touch. I really need a pulse of the labs about who is up and running, who has shortages and of what.”
March 13, 2020: Michael Ettinger, a senior vice president at medical supply company Henry Schein, emailed Giroir. He said, “Henry Schein has identified 3 companies that have filed EUAs [emergency use authorizations] for lateral flow quick tests and nasal swab tests. […] We can have 40,000 tests on Monday, 1 million tests a week from now, and then in April we can ramp up to 1 million tests per day.” He continued, “Henry Schein is prepared to respond to the government’s call to action and partner to alleviate the urgent need for wide availability of rapid testing.” Giroir replied, “received.”
In late March, Henry Schein announced the availability of rapid tests and said it planned to distribute them. But in April, the United States was only testing an average of 140,000 people a day — far below the 1 million mark.
Also on March 13, Matthew Johns, an HHS Region IX administrator, sent an email about testing in the Bay Area. Trent-Adams replied, “Your assistance will be greatly appreciated. Your knowledge of the region and local area will help get this moving as we tackle this challenging situation.”
March 14, 2020: Julie Khani, the president of the American Clinical Laboratory Association, emailed Paul Mango, the deputy chief of staff for policy at HHS, with projected supply needs that included 96,000 N95 respirators and 3 million masks. This was forwarded to Kadlec.
Testing Problems
Feb. 7, 2020: Perkins and Karin Von Eije, a virologist at WHO, sent an email with the subject line “Information for 2019-nCoV expert network.” The email noted that both the WHO and the CDC were distributing Covid-19 tests. They also wrote that for the CDC test, orders were limited to one kit per national lab because only a limited number of kits were available.
Feb. 14, 2020: Darin Carroll, director of the CDC’s Environment, Safety and Health Compliance Office, said, “We were made aware this morning that there will be 350 swab sets … coming in as early as Monday. In order to get these done in the timeframe that will likely be set for us, we need to think through how the work load can be divided between the Respiratory virus lab and [the Clinical and Environmental and Microbiology Branch]..” Lindstorm replied, “We can work to manage the surge.”
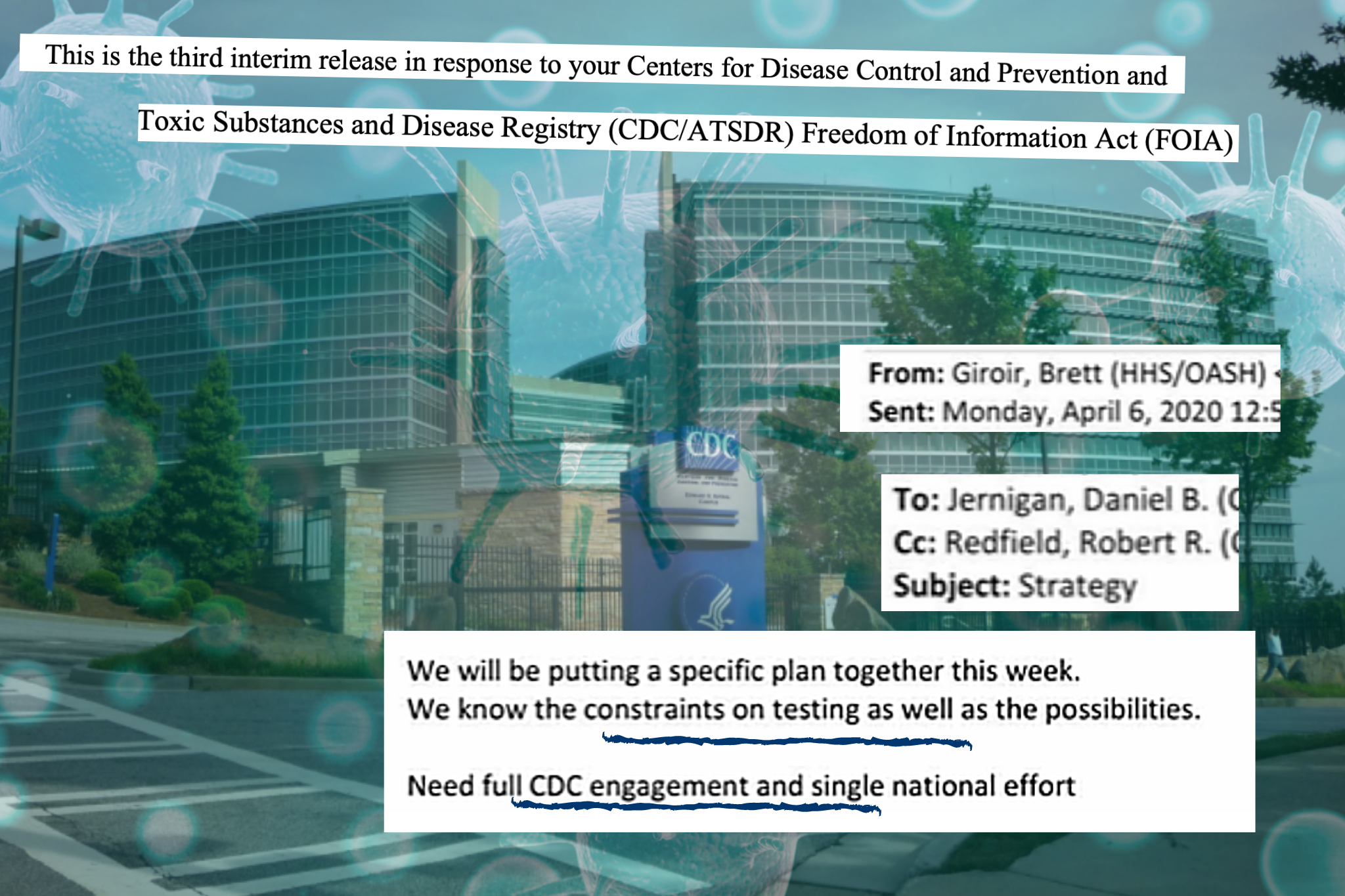
March 7, 2020: Giroir sent an email with the subject line “Please Confirm,” saying, “While there were the issues with the distributed tests, CDC (and perhaps a few other labs like Nebraska) were still doing testing. So if a person truly needed a test, they got it. No matter where they were.” Schuchat’s reply is almost entirely redacted, except for the phrase “I don’t think.”
March 15, 2020: In an email about a White House task force news conference that day, Schuchat wrote that it “included messaging about the usphs-fema partnership on setting up drive by screening. … They stated that the priority of this screening was for health care workers, responders, and people who are immunocompromised or elderly and they were requesting that others stand by and help let those people be prioritized.” Joe Bresee, the director of the CDC’s Influenza Division, said that he “like[d] the messaging for focus on high risk groups.” Schuchat replied, “Yes it was a relief to me that at least something practical was announced.”
March 16, 2020: Rebecca Avitia, New Mexico Sen. Heinrich’s chief of staff, emailed Schuchat, “[W]e have a laboratory in New Mexico with the capacity to run 9,000 tests per day (thereby scaling the entire region’s ability to test), but they are not able to do so because Roche has limited the reagent they will supply, purportedly according to CDC and FDA guidelines.” When discussing the message with other CDC officials, Schuchat said, “I heard from Dr Giroir he had spoken w the New Mexico governor’s office.” Jay Butler, the deputy director for infectious diseases at the CDC, replied, “I can give the staffer a call.”
Communications with States and Private Companies
Feb. 23, 2020: There was a call between U.S. corporation 3M and multiple government officials, including Kadlec, FDA Commissioner Stephen Hahn, and Steven Adams, the deputy director of the Strategic National Stockpile Program. An email sent by HHS official David Hassell before the meeting with a summary of facts about decontamination and reuse of N95 masks said, “Bottom line is that they cannot be effectively decontaminated for reuse.” Depleted N95 supplies have led to these masks being reused during the pandemic.
Feb. 25, 2020: Ajay Royan, the managing partner of Mithril Capital Management, a firm founded by Peter Thiel that was investigated by the Federal Bureau of Investigation, sent an email introducing Adimab, a company that researches antibodies and assisted during the Ebola crisis. Giroir looped in Bright, who asked Adimab to submit its information to a portal for the Medical Countermeasures Task Force and connected Royan with John Tegeris, the program manager for BARDA’s CoronaWatch program.
Feb. 28, 2020: Darcie Johnston, the HHS director of intergovernmental affairs, sent an email detailing specific needs of the governor of Arkansas. She wrote: “The Governor spoke with Vice President Pence today. He asked the VP for 2 things: 1. The ability to have state-level testing so they do not have to send samples to the CDC. The VP told the Governor the state should have that next week. 2. An adequate supply of PPE for future needs. The VP mentioned that the federal government is looking at emergency authorities to ensure this.”
Despite these promises, on March 6, Arkansas’ testing capacity remained extremely limited — the state could test only four or five people per day. And critical PPE shortages throughout March put thousands of doctors at risk.
Also on Feb. 28, Johnston sent an email with the subject line, “Governors request.” Keagan Lenihan, the chief of staff at the Food and Drug Administration, replied, “We can’t give specifics on shortages.”
March 8, 2020: Various officials at HHS and at the Centers for Disease Control and Prevention, including Giroir, Kadlec, and Yeskey, had a call with Kaiser Permanente and HCA Healthcare.
March 11, 2020: Former DHS Secretary Kirstjen Nielsen pitched ANDE, a corporation specializing in rapid DNA technology with long-standing government ties, to help with Covid-19 testing. She wrote to HHS Secretary Alex Azar, “I know about them b/c I had hoped we could deploy rapid DNA technology on our southern border for a variety of reasons.”
March 13, 2020: Giroir offered Louisiana Gov. John Bel Edwards White House assistance with setting up drive-through testing sites, which Edwards accepted. Edwards then said, “I am afraid the testing is nowhere near as robust as necessary to identify more positive cases that can then be isolated/quarantined so that we can in a significant way slow the spread, flatten the curve, and better ensure that our medical/hospital capacity is not overwhelmed. Please make every effort to significantly increase our testing capacity and testing through put as soon as possible.”
March 16, 2020: Stephen Tang, the CEO of OraSure, sent Giroir a proposal for at-home Covid-19 tests. Giroir copied Bright and Jeff Shuren, the director of the Center for Devices and Radiological Health on this reply, saying, “How can I help?” Shuren’s and Bright’s replies are redacted.
Also on March 16, Cimarron Buser, the senior vice president of TimeTrade, emailed Donald Rucker, the HHS national coordinator for health information technology, with a proposal for software that could schedule Covid-19 testing appointments. This was forwarded to Giroir and Kadlec.
March 17, 2020: Udit Batra, the CEO of MillporeSigma, sent Giroir an email pitching his company for Covid-19 test and vaccine manufacturing. Giroir forwarded this to Shuren.
Conversations About Press Coverage
Feb. 21, 2020: Tara Broido, the deputy director of communications at HHS, sent a Politico article entitled “White House fears coronavirus could shape Trump’s 2020 fortunes” to Giroir and others in his office. Giroir sent a reply, which is redacted. Mia Heck, director of external affairs in Giroir’s office, responded, “Copy.” Giroir sent another reply, which is also redacted.
Feb. 27, 2020: Broido sent a Washington Post article entitled “Workers without protective gear or proper training met coronavirus evacuees, HHS whistleblower says” to Giroir and others. Giroir replied, “Exactly what the department needs today!!!”
Feb. 29, 2020: Giroir circulated a press release on three patients in Washington state who tested positive for Covid-19, including one who had died. Giroir said, “There is 100% chance that the remaining 50+ all have COVID and that we can expect even more to become ill soon.”
March 12, 2020: Elisabeth Handley, interim director of the Office of Research and Integrity at HHS, forwarded to several people a message from the National Treasury Employees Union entitled “HHS Silence on Coronavirus Puts Employees at Risk.” Trent-Adams forwarded it to Deputy Assistant Secretary Valentine.